OVERVIEW
Introduction : the cancer of esophagus is the neoplasia of the tube digestive of worse prognosis. Their treatment constitutes a challenge to the treat is of patients with deterioration nutritional with inability of swallowing food. The majority are tributaries of treatment palliative.
Objective: describe the experience in it attention nutritional of them patients with cancer of esophagus and Cardia with the introduction of the Group of support nutritional in the Hospital Universitario “Commander Manuel Fajardo”.
Method: is present 126 sick with cancer of esophagus and Cardia, 51 of them with injuries resectable to which is performed esophagectomy and 75 sick with cancer advanced e interventions palliative, served from 2006 until 2015, according to them protocols of action of the Group of support nutritional.
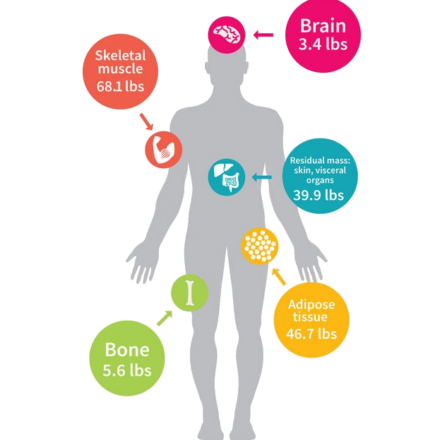
Results: all them patients is were between 46 and 76 years, 69% greater of 60 years, 87.3% of the sex male, 90% with a history of smoking and 80% of alcoholism. The location of the tumor predominated in the a lower third of the esophagus and Cardia, followed by the upper third and middle third. Presented malnutrition mild 4.1%, 53.9% moderate and 42% serious. All presented reduction of the albumin and 57.9%, the capacity functional decreased. All received counseling dietary and diet therapy oriented. Is increased the survival in 14 months in those cases palliative and to 39 months in them resectivos, compared with a period earlier without the presence of the Group of support nutritional.
Conclusions: nutritional assessment should be part of the clinical evaluation of patients with cancer of the esophagus from the time of diagnosis and during the illness, in order to identify and correct nutritional deficit, maintain and preserve weight. This improves the response to the different oncological treatments, increases survival and improves quality of life.
INTRODUCTION
Cancer of the esophagus and Cardia, is neoplasm of the digestive tract of worse prognosis by its late prescription and deterioration of the nutritional status, your treatment is a great challenge and in the majority of patients is palliative. 1-5 the malnutrition is present in 79% of the cases before starting treatment. 3-4 our objective is to describe the experience in the care and nutritional management of patients with cancer of the esophagus and Cardia with the introduction of the Group nutritional support (GAN) in the University Hospital Commander Manuel Fajardo.
METHODS
Is conducted a study observational, analytical, prospective of cutting transversal, type series of cases of them sick with cancer of esophagus and Cardia served in the period from 2006 to 2015. The universe and sample of the work was made up of 126 patients where he participated the nutritional support group (GAN) created in 2005 to define and implement the programs alimentaria-nutrimental and metabolic intervention of hospitalized patients. Inclusion criteria were the diagnosis, histological confirmation and the attention of the GAN. This included clinical aspects, anthropometric parameters (weight, height, and BMI), biochemical (blood count with differential, total protein, albumin, blood glucose, creatinine and colesterol) immune (lymphocyte count = Total leukocytes x % of lymphocytes / 100) and functional (such as measuring the force non-dominant hand), type of nutritional intervention and survival.
The survey of assessment global subjective (VGS) of the State nutritional allows classify them categories of malnutrition and establish the modality nutritional:
Mild: Loss of body weight (PPC) the 6 months prior to diagnosis between 0-5%, BMI (BMI) 20-25 kg/m2 lymphocyte count higher than 1 500 linfos/mm3 and top 35 g/l albumin).
Moderate: 10-20% PPC, BMI 16 – 17 kg/m,2 reduction of the intake of food in recent weeks, loss of subcutaneous tissue, cells of 800-1 200 linfos/mm3 and albumin between 28-31 g/l .
Grave: PPC greater than 20%, BMI less than 16 kg/m,2 severe loss of muscle mass and subcutaneous tissue, the presence of oedemas, lymphocytes inbotto 800 linfos/mm3 and below 28 g/l albumin.
RESULTS
The age varied from 46-76 years with an average of 63 years, predominated the sex male (87.3%), in 48% there were diseases chronic. History of smoking, there were 90% and 80% alcohol. The dysphagia, loss of weight and swallowing pain was present in 68%. The location more frequent of the tumor was in a third bottom of the esophagus and Cardia 50%, 40% in third half and 10% in the top. In stage II, 7%; in the III, 53% and in the IV, 40%. According to BMI, 42% had severe malnutrition, 53.9% moderate and mild 4.1%. 58.7% with decreased functional ability (table 1). In all the patients was decreased the albumin and at 57.9% the cholesterol. In 48.4% were decreased the lymphocytes, with predisposition of an infection (table 2).
All the patients received valuation e intervention nutritional with counseling dietary and diet therapy oriented with supplements, support enteral by jejunostomy and power oral after placement of prosthesis in the cancer advanced, with follow-up and monitoring nutritional. The nutrition parenteral is employed in patients malnourished and nutrition mixed, parenteral and enteral, before the surgery and the postoperative, to start the feeding oral (table 3 )).
An increase in survival was achieved up to 39 months in tumors unresectable, exceeding the period without the GAN (table 4 and 14 months in advanced cancer).
DISCUSSION
Cancer risk factors of esophagus stands out the ingestion of alcoholic drinks, smoking and ingestion of carcinogens such as nitrites, opiates smoked and certain mycotoxins. 2,3,6-7 to the diagnosis, 40%-80% present malnutrition, increase of morbidity, mortality, time of hospitalization and failures therapeutic. 7-12
The diet with fruits and vegetables has a protective effect and obesity increases the risk of disease by reflux and esophageal Barret. 13-16 weight is a nutritional indicator, weighing less than 10% of the ideal weight and one further 10% loss is associated with increased risk of complications. The treatment of the loss of weight produces improvement of the survival and decrease of complications. BMI expresses the loss of weight in relation to height. The malnutrition serious has impact on the system immune, was present in 40% of the series. 17-21
Between those markers nutritional, highlights the concentrations plasma of proteins visceral, synthesized in the liver, as measurement of the mass protein body. Them proteins somatic as it creatinine serum for determine the mass muscle and the number of lymphocytes, to evaluate the response immune, the decrease of cholesterol is associated to increase of the risk of mortality in elderly. 21 In the visceral protein assessment we use the total proteins and albumin, a decreased albumin allows you to set the malnutrition, but in short periods, by its half-life of 14 to 21 days.
The total lymphocyte count is a nonspecific indicator of the State of immunocompetence and measures the ability to mobilize cells inmunoactivas to face the aggression. One lymphocyte count less than 1 500 cells/mm warning risk of sepsis. Serum albumin and lymphocyte predict complications post-surgery, of being low, the probability of complication is 90%. The stadium and the dysphagia duration determines the magnitude of the nutritional loss and inappropriate feeding leads to a nutritional energy malnutrition (DEN) with thinning. The frequency and degree of DEN is linked to the type of tumor, stadium and the plan cancer. 21 The majority of patients referred to dysphagia, odynophagia and weight loss. 22-33 Loaeza and Villalobos observed dysphagia (87-97%), loss of weight (96-100%), heartburn (30-55%), odynophagia (21-30%), hemorrhage (17-21%), aspiration into lungs (7-17%), pain abdominal (24-26%) and fatigue (14-48%). 9
Before start it nutritional perform assessment of the State of health, type of tumor, State nutritional, response predictable and its capacity and predisposition to face the situation, for determine the risk e start these measures nutritional. Methods vary from modification of diet, food supplements, enteral and intravenous feeding, dietary history, anthropometric measurements, the laboratory tests, calculation of nutritional requirements and dietary assessment. Nutritional therapy goals are: avoiding or reversing nutrient deficiencies, conserve body mass, help to tolerate treatments, reduce side effects and complications, maintain the strength and power, protect immune function, reduce the risk of infection, assist in the recovery and improve the quality of life. Cachexia is a vital threat more immediate than the local effects of the tumor. 17-21 in the cancer advanced, the goal nutritional is the relief of them symptoms,21 that the sick is capable of incorporate is of the bed, clean is, dress is and approach is to a better quality of life. It 21 surgery is the main treatment in early stages, (Tis-T1a N0) with a radical operation (esophagectomy and a regional lymphadenectomy) and in the advanced tumor treatment is palliative,1,4,22-25,34,35 directed to the relief of the obstruction – causes of malnutrition and morbidity and mortality-36-39 increase tolerance to chemo-radiotherapy, offer well-being and improve the quality of life.
He development of way of access, nutrients and equipment interdisciplinary enable that them patients leave the hospital and are reintegrated to the life family with a quality acceptable. 18,21 In our protocol is includes the support nutrition adequate and evaluation of the risk surgical independent if the tumor is resectable or not. The definitive food Ostomy (Gastrostomy or jejunostomy), were considered a last option procedure, by its ethical problem. 30-31 assessment and nutritional support allowed an adequate preparation in patients with resectable lesions, improve the nutritional status and reduce postoperative complications. In them cancers advanced, are provided an intervention food, avoiding the loss quick of weight which reversed the malnutrition, to the be favored by Ostomy food, implantation of prosthesis and power parenteral or mixed. The placement of an esophageal transtumoral prosthesis was possible in all patients.
Patients with esophageal cancer are a challenge usually advanced state of nutritional deterioration in that query. Is important it evaluation clinical of the State nutritional from the diagnosis for correct the deficit nutritional, provide a via of power enteral early, reduce the loss of weight, avoid them effects side of the malnutrition, improve the response to the treatment, decrease them complications, decrease the cost hospital, increase the survival and the quality of life.
Conflict of interest
The author does not represent conflicts of interest.
REFERENCES
- mederos Curbelo ON, loyal Mursuli, García Gutiérrez, Barrera Ortega JC, Valdes Jimenez J, Romero Diaz CA. What they do and what we do in esophagus and Cardia cancer. Rev Cubana Cir. 2005; 44 (4). Available at: http://scielo.sld.cu/scielo.php?script=sci_arttext & pid = S0034-74932005000400010 & lng = en & nrm = iso & tlng = is
- Enzinger PC, Mayer RJ. Esophageal Cancer. NEJM. 2003; 349:2241-52.
- Mc Quaid KR. Injury esophageal malignant. In: Mcphee SJ, Papadakis MA, Tierney LM. Clinical diagnosis and treatment. 39 ed. Mexico: the Manual modern; 2005:547-9.
- Ayre AM, Fernández A, Coco JE. Treatment of the cancer of esophagus: review. Journal of graduate of the Chair of Medicine [on line]. 2003 [cited 15 may 2012]; 126:37-41. Available at: http://www.med.unne.edu.ar/revista/revista126/tratamiento.htm
- barriers Ortega JC, Mederos Curbelo ON, Romero Diaz CA, Cantero Ronquillo to, of the camp Abbot RJ, Valdes Jimenez J. Cancer not resectable of esophagus and Cardia. Prosthesis or tube gastric? Arch Cir Gen Dig. 2005 [cited may 15, 2012]; 44 (4). Available at: http://www.cirugest.com/revista/2005/02/2005-01-24.htm
- Cancer of the esophagus. In: Diseases and treatments. Available at: http://www.cun.es/areadesalud/enfermedades/cancer/cancer-de-esofago/
- Eslick GD. Epidemiology of esophageal cancer. Gastroenterol Clin North Am. 2009;38:17-25.
- Tomizawa Y, Wang K. Screening, Surveillance, and Prevention for Esophageal Cancer. Gastroenterol Clin North Am. 2009;38:59-73.
- Loaeza-del Castillo A, Villalobos-Pérez J. Estudio de 30 años sobre el cambio en la frecuencia de carcinoma epidermoide esofágico, adenocarcinoma esofágico y adenocarcinoma de la unión esofagogástrica. Rev Gastroenterol Mex. 2008;73(1):11-6.
- Goyal RK. Disease of the Esophagus. En: Kasper DL, Braun Wald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, ed. Harrison’s Principles of Internal Medicine. 16 th Edition. New York: McGraw-Hill; 2005. p. 1739-1743.
- Klag MJ. Digestive Disease Library Esophagus Cancer. TJH MIGH [en línea] 2007 [Citado 22 de diciembre de 2006]. Disponible en: http://hopkinsgi.nts.jhu.edu/pages/latin/templates/index.cfm?pg=disease1&organ=1&disease=14&l
- Lacy BE, Weiser K, Chertoff J. The diagnosis of gastroesophageal disease. Am J Med. 2010;123:583-92.
- Rastogi A, Puli S, El Serag HB. Incidence of esophageal adenocarcinoma in patients with Barrett`s esophagus and high grade dysplasia: a meta-analysis. Gastrointest Endosc. 2008;67:394-98.
- Sharma P, Falk GA, Weston AP. Dysplasia and cancer in a large multicenter cohort of patients with Barrett`s esophagus. Clin Gastroenterol Hepatol. 2006;4:566-72.
- Updated guidelines 2008 for the diagnosis, surveillance, and therapy of Barrett`s esophagus. Am J Gastroenterol. 2008;103:788-97.
- Seewald S, Ang TL, Soehendra N. Endoscopic mucosal resection of Barrett’s esophagus containing dysplasia or intramucosal cancer. Postgrad Med. 2007;83:367-72.
- Murphy PM, Modi P, Rahamim J. An investigation into the current peri-operative nutritional management of oesophageal carcinoma patients in major carcinoma centres in England. Ann R Coll Surg Engl. 2006;88:358.
- Hoda D, Jatoi A, Burnes J. Should patients with advanced, incurable cancers ever be sent home with total parenteral nutrition. Cancer. 2005;103:863.
- Lecleire S, Di Fiore F, Antonietti M, Ben Soussan E, Hellot MF, Grigioni S. Undernutrition is predictive of early mortality after palliative self-expanding metal stent insertion in patients with inoperable or recurrent esophageal cancer. Gastrointest Endose. 2006;64:479-84.
- Pultrum BB, van Westreenen HL, Mulder NH, van DuUemen HM, Plukker JT. Outcome of palliative care regimens in patients with advanced oesophageal cancer detected during explorative surgery. Antieaneer Res. 2006;26:2289-93.
- Rocabruna Pedroso R. Nutrición en cirugía. Rev Cubana Cir. 2009;48(1). Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-74932009000100016&lng=es&nrm=iso&tlng=es
- National Cancer Institute. Cancer of the esophagus: treatment. INC [Online] 2007 [cited 15 may 2012]. Available at: http://www.cancer.gov/espanol/pdq/tratamiento/esofago/
- Politi PM. Cancer of esophagus: alternatives to the surgery in the year 2007. Results to long term. [Online], 2007 [cited 3 of May 2007]. Available at: http://www.cancerteam.com.ar/poli181.htm
- dug D. treatment surgical of the cancer of esophagus. AAC [on-line] 2006 [cited 23 April 2007]. Available at: http://www.aac.org.ar/Pdf/ut0702.pdf
- kills to, Llach J, Bordas JM. Treatment palliative of the cancer of esophagus. GHC [Online] 2007 [cited may 15, 2012 in]; 6:68-71. Available at: http://www.ghcontinuada.com/contenidos/pdf/v6n2a398 pdf001.pdf
- Oñate OLF, Milan RG, Aiello CV, Carrillo JF, Gallardo RD, Brom-Valladares R. Treatment of the adenocarcinoma of the esophagogastric junction at a single institution in Mexico. Ann Surg Oncol. 2007; 14:1439-48.
- Lagarde SM, Ten Kate FJW, Reitsma JB, Busch ORC, Van Lanschot JB. Prognostic factors in adenocarcinoma of the esophagus or gastroesophageal junction. J Clin Oncol. 2006; 24 (26): 4347-55.
- Besharat S, Jabbari to, Semnani S, Keshtkar A, Marjani J. Inoperable esophageal cancer and outcome of palliative care. World J Gastroenterol. 2008; 14 (23): 3725-8.
- Keller R, Flieger D, Fischbach W, Christi SU. Self-expanding metal stents for malignant esophagogastric obstruction: experience with a new design covered nitinol stent. Gastrointestin liver Dis. 2007;16:239-43.
- Barrera Ortega JC, Mederos Curbelo ON, Da Costa Fernández JM, Gigato Díaz A. Efectividad del alcohol absoluto para canalizar los tumores irrresecables de esófago. Rev Cub Cir. 2010;49(4):9-14.
- Barreras Ortega JC, Mederos Curbelo ON, Romero Díaz C, Cantero Ronquillo A, Menchaca Díaz JL, Castellano JA. Estrategia en el cáncer de esófago torácico y cardias irresecable. Rev Cub Cir. 2001;40(2):119-22.
- Conigliaro R, Battaglia G, Repici A, De Pretis G, Ghezzo L, Bittinger M. Polyflex stents for malignant oesophageal and oesophagogastric stricture: a prospective, multicentric study. Eur Gastroenterol Hepatol. 2007;19:195-203.
- Javle M, Ailawadhi S, Yang GY, Nwogu CE, Schiff MD, Nava HR. Palliation of malignant dysphagia in esophageal cancer: a literature-based review. Oncol. 2006;4:365-73.
- Mederos Curbelo ON, Barreras Ortega JC, Romero Diaz CA, Cantero Ronquillo A, Menchaca Diaz JL. Bypass gástrico tubular isoperistáltico (Postlethwait) en el cáncer de esófago irresecable. Rev Cubana Oncol. 2001;17(2):135-7.
- Law S, Wong J. The Current Management of Esophageal Cancer. Adv Surg. 2007;41:93-119.
- romero Diaz C, Mederos Curbelo ON, Barrera Ortega JC, Valdes Jimenez JM, Cantero Ronquillo A. surgery Oncology. Best quality of life in esophageal cancer. Magazine advances medical of Cuba. 2000; 24 (4): 50-2.
- Tate H. The Palliation of Dysphagia in Oesophageal Malignant Obstructions Using Endoprostheses: A Review of the Literature. Newcastle upon Tyne: Priory Lodge Education Ltd; 2007.
- Fernández Aguilar M, Manrique Rionda E, Marchena Pérez E. survival of two patients with inoperable esophageal cancer treated with endoscopic recanalization. Medicentro electronic. 2008; 12 (2): 62-4.
- cross-Zárate to, Hernandez-guerrero to, nephew-Cossío S, ravine-Fragoso B, Alonso-Larraga JO. Survival and factors prognoses in cancer esophageal. Revista Médica of the General Hospital of Mexico. 2010; 73 (1): 23-9.
-
Oliva Anaya, Carlos Antonio, et al. “Soporte nutricional y calidad de vida en pacientes con cáncer de esófago y cardias.” Revista Cubana de Cirugía 55.2 (2016): 0-0.
 NL
NL FR
FR DE
DE EN
EN